Journal of Nutrition Research
An official journal of IAPEN India association
Journal of Nutrition Research
DOI: 10.55289/jnutres/v12i2.43
Year: 2024, Volume: 12, Issue: 2, Pages: 75-85
Review Article
Shivshankar Timmanpyati1∗, Eileen Canday2, Bhakti Samant3, Varsha Gorey4, Shilpa Chadha Thakur5, V Prashanthi Suryanarayana6, Tiash Sinha7, Shruti Bhardwaj8, Rajeshwari Prem9, Dimi Ingtipi10
1Dietician, Tata Memorial Hospital, HBIN, Mumbai, Maharashtra, India
2Head of Department (Nutrition & Dietetics), Sir H. N. Reliance Foundation Hospital and Research Centre, Mumbai, Maharashtra, India
3Chief Clinical Dietician, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, Maharashtra, India
4Senior Clinical Dietitian, Apollo Hospitals, Navi Mumbai, Maharashtra, India
5Senior consultant, Dietetics Asian Hospital, Delhi, India
6Chief Dietitian, induscancer.com, Basavatarakam Indo American Cancer Hospital & Research Institute, Hyderabad, Telangana, India
7Senior Clinical Nutritionist, Tata Medical Center, Kolkata, West Bengal, India
8Chief Clinical Nutritionist, Zydus Hospitals, Ahmedabad, Gujarat, India
9Dietitian, Homi Bhabha Cancer Hospital and Research Centre, Vizag, Andhra Pradesh, India
10Assistant Dietitian, Dr. B. Borooah Cancer Institute, Guwahati, Assam, India
*Corresponding Author
Email: [email protected]
Received Date:13 December 2024, Accepted Date:28 December 2024, Published Date:30 December 2024
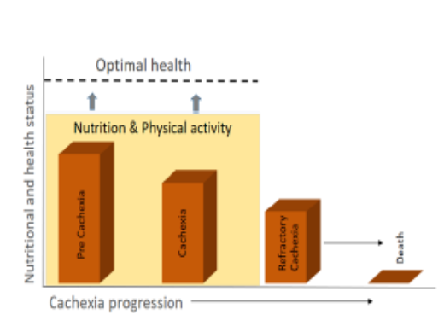
Cancer cachexia is a multifactorial syndrome marked by progressive weight loss, muscle wasting, and systemic inflammation, commonly associated with advanced cancer. Its management poses a significant challenge due to the complex interplay of metabolic alterations, reduced appetite, and inflammation. Addressing the nutritional needs of patients with cachexia is a cornerstone of care, aiming to mitigate weight loss, preserve lean body mass, and enhance quality of life (QOL). Effective nutritional strategies include individualized meal plans enriched with energy-dense and protein-rich foods, alongside the use of specialized nutritional supplements. Pharmacotherapy, such as appetite stimulants, anabolic agents, and anti-inflammatory drugs, plays a crucial role in modulating metabolic dysfunction and supporting nutritional goals. Additionally, physical activity tailored to the patient's abilities has been shown to complement nutritional and pharmacological interventions by promoting muscle retention and functional independence. A multidisciplinary approach that integrates dietary support, pharmacotherapy, and exercise is essential for optimizing outcomes in cancer cachexia management and improving patient well-being.
Keywords: Cancer cachexia, Nutritional management in cancer, Malnutrition in cancer
© This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By India Association for Parenteral and Enteral Nutrition (IAPEN)
Subscribe now for latest articles and news.