Journal of Nutrition Research
An official journal of IAPEN India association
Journal of Nutrition Research
DOI: 10.55289/jnutres/v12i2.47
Year: 2024, Volume: 12, Issue: 2, Pages: 110-122
Original Article
B Ravinder Reddy1, Sambit Sahu2, C V Kiran Kumar Reddy3, Rachana M Bhoite4∗, Praneeth Immadisetti5, Rayees Unnisa6, Arti Sanghavi7, Vinita Satyavrat8
1 Sr. Consultant, Gastroenterology - Surgical, General Surgery, CARE Hospitals, Banjara Hills, Hyderabad, Telangana, India
2 Medical Director, HOD-Critical Care, KIMS Hospitals, Secunderabad, Begumpet, Telangana, India
3 Deputy Medical Superintendent, KIMS Hospitals, Begumpet, Secunderabad, Telangana, India
4 Head-Nutrition Science and Clinical Research, India & Emerging Markets, Dr Reddy’s Laboratories Limited, Ameerpet, Hyderabad, Telangana, India
5 Nutrition Scientist-Nutrition Science and Clinical Research, India & Emerging Markets, Ameerpet, Dr. Reddy’s Laboratories Limited, Hyderabad, Telangana, India
6 Team Member-Medical Affairs, Dr. Reddy’s Laboratories Limited, Ameerpet, Hyderabad, Telangana, India
7 Team Lead-Clinical Research, Medical Affairs, Dr. Reddy’s Laboratories Limited, Ameerpet, Hyderabad, Telangana, India
8 Head, R&D & Medical Affairs, Nutraceuticals, Dr. Reddy’s Laboratories Limited, Ameerpet, Hyderabad, India
*Corresponding author
Email: [email protected]
Received Date:23 December 2024, Accepted Date:30 December 2024, Published Date:31 December 2024
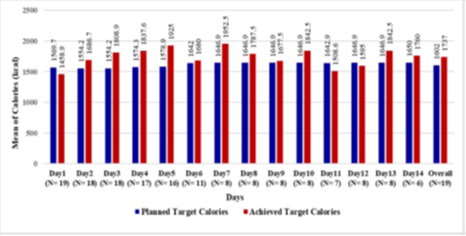
Enteral Nutrition (EN) prevents malnutrition and promotes recovery in critically ill patients. Despite the benefits, current EN formulations are associated with concerns like gastrointestinal intolerance, electrolyte imbalances, and hyperglycemia. Balanced EN formulations improve recovery, reduce hospital stays, and enhance patient outcomes. This study evaluated efficacy and tolerability of a novel balanced EN formula in supporting patient recovery and reducing length of hospital stay in critically ill patients. The study included 19 hospitalized critically ill patients aged ≥18 years, with mean (SD) age of 52.4(14.98) years. EN intake was monitored for a minimum of 3-14 days or until discharge. Target calorie and protein intakes were evaluated in accordance with ASPEN/ESPEN guidelines 2019. The analysis of target macronutrient intake reported adequate levels in 17 (89.5) patients, with a mean (SD) daily caloric intake of 1737 (582.1) kcal, and 95% Class Interval (CI) ranging from 1646 to 1828 kcal. The mean (SD) of daily protein intake was 82.9 (27.78) grams. The mean (SD) hospital stay was 12.7 (9.39) days, with a Interquartile range (IQR) of 11 (7.0;18.0) days and a median of 8 days. Most patients showed improvements in micronutrient profiles and achieved electrolyte homeostasis without hyperglycemic episodes. Notably, no gastrointestinal (GI) complications were observed, and no prokinetic agents were administered, indicating tolerability and acceptance of the formula. No serious adverse events (SAEs) were reported. These findings suggest that the novel EN formula is effective in supporting the recovery of critically ill patients, while demonstrating favourable safety and tolerability profile.
Keywords
Critical Illness, Nutritional Support, Enteral Nutrition, Macronutrients, Micronutrients, Gastrointestinal Tract, Feed Tolerance, Prokinetics, ESPEN Guidelines
© This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By India Association for Parenteral and Enteral Nutrition (IAPEN)
Subscribe now for latest articles and news.